Is mechanical ventilation exacerbating the COVID-19 death toll?
A recent WebMD article reported that a 90 year old woman, hospitalised due to a COVID-19 infection, had refused to be put on a ventilator and survived.
This report refreshed my recollection that commonly some 25% of those subjected to a mechanical ventilator succumb to ventilator associated pneumonia caused by a secondary infection.
Although the cause for a ventilator-associated secondary infection is commonly ascribed to be due to microbes infiltrating into the lungs because of the presence of a hollow tube (artificial airway) that goes in the mouth and down into the main airway or trachea and is connected to the ventilator, there are other factors to consider.
Members of a research group that was part of over a decade ago hypothesised mechanical positive pressure ventilation subjects the lungs to unnatural pulses and pressures of air going into the lungs that compromise the integrity of the lungs, not only on a macro level but also at a molecular level.
This is because it disrupts the phospholipid protein complex which covers the whole respiratory surface which contributes to sustaining simultaneously proper respiratory gas exchange and offers mechanical stabilization under the dynamic conditions imposed by breathing, and protection against the pathogenic invaders surface, according to Pérez-Gil Biochimica et Biophysica Acta in Biomembranes (2008).
Recent reports question the use of ventilators with COVID-19 patients and are opting for alternatives, such as nasal oxygen supplementation.
What was known about the risks of using mechanical ventilation prior to its use in COVID-19 Patients?
Koenig et al reported in Clin Microbiol Rev in 2006 “that patients in the intensive care unit (ICU) are at risk for dying not only from their critical illness but also from secondary processes such as nosocomial infection.
Pneumonia is the second most common nosocomial infection in critically ill patients, affecting 27% of all critically ill patients (170). Eighty-six percent of nosocomial pneumonias are associated with mechanical ventilation and are termed ventilator-associated pneumonia (VAP).
Between 250,000 and 300,000 cases per year occur in the United States alone, which is an incidence rate of 5 to 10 cases per 1,000 hospital admissions (134, 170). The mortality attributable to VAP has been reported to range between 0 and 50% (10, 41, 43, 96, 161).
Studies have provided different results when determining attributable mortality, in part because of very different populations (less-acute trauma patients, acute respiratory distress syndrome [ARDS] patients, and medical and surgical ICU patients) and in part as a result of variances in appropriate empirical medical therapy during the initial 2 days.
Furthermore, the organisms recovered have an impact on outcome, with higher mortality rates seen in VAP caused by Pseudomonas aeruginosa, Acinetobacter spp., and Stenotrophomonas maltophilia (109). Beyond mortality, the economics of VAP include increased ICU lengths of stays (LOS) (from 4 to 13 days), and incremental costs associated with VAP have been estimated at between $5,000 and $20,000 per diagnosis (20, 206, 211).
Ventilator-associated pneumonia is defined as pneumonia occurring more than 48 h after patients have been intubated and received mechanical ventilation. Diagnosing VAP requires a high clinical suspicion combined with bedside examination, radiographic examination, and microbiologic analysis of respiratory secretions.
Aggressive surveillance is vital in understanding local factors leading to VAP and the microbiologic milieu of a given unit. Judicious antibiotic usage is essential, as resistant organisms continue to plague intensive care units and critically ill patients.
Simple nursing and respiratory therapy interventions for prevention should be adopted. Over the past several decades our understanding of VAP has grown significantly with regard to pathogenesis, risk factors, diagnostic testing, therapies, and prevention by modifying risk factors. This paper is designed for the practicing clinician in addressing diagnosis, treatment, and prevention of VAP.”
Government departments are aware of ventilator –associated pneumonia, SA Health updated its information on Ventilator–associated pneumonia prevention on the 21st of April and reports that up to one quarter of patients requiring mechanical ventilation develop ventilator associated pneumonia.
It notes that ventilator-associated pneumonia can be caused by the migration of microorganisms from colonised endotracheal and/or tracheostomy tubes, direct inoculation via bronchoscopy or other respiratory procedures or by aspiration. Affected patients may have prior underlying lung disease or immune suppression.
How were ventilators to be used for COVID-19 patients?
A joint statement found at Queensland heath recommends that early recognition and referral of patients with worsening respiratory function while on conventional oxygen therapies such as simple face masks or masks with reservoir bags is important to ensure timely and safe escalation of respiratory support.
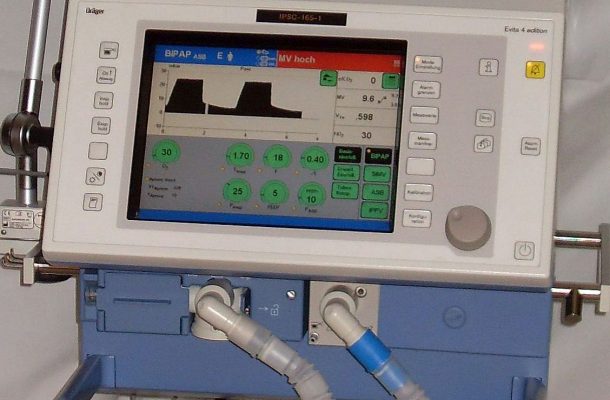
Early optimisation of care and involvement of Intensive Care Unit (ICU) is recommended. The therapies can be considered in caring for COVID-19 patients includes lung protective mechanical ventilation (MV) for management for acute respiratory failure.
Mechanical ventilation should be employed with the use of a low tidal volume strategy (4-8ml/kg predicted body weight) and limiting plateau pressures to less than 30 cmH2O. Permissive hypercapnia is usually well tolerated and may reduce volutrauma.
Higher levels of PEEP (positive end-expiratory pressure ,greater than 15 cmH2O) are recommended. Alternate modes of ventilation such as APRV (airway pressure release ventilation) may be considered based on clinician preference and local experience. Viral (rather than HME) filters should be utilised, and circuits should be maintained for as long as allowable (as opposed to routine changes).
Reports on the use of ventilators and the risk of secondary infections
A recent report in Scientific American Blogs specifically addresses the increased risk of secondary infections to high-risk COVID-19 patients that end up in critical care on ventilators for an extended period of time.
The SAB reports that bacterial co-infections such as pneumonia pose a serious threat to high-risk COVID-19 patients, with many factors coming together to create severe, life-threatening and, in some cases, deadly complications that cannot be ignored by the health care community.
Most at-risk are older adults and those with pre-existing conditions as they’re more likely to be hospitalized for longer periods of time and require use of medical devices such as ventilators.
When these high-risk individuals end up in critical care, they are more likely to stay there for an extended period of time, increasing the risk for exposure to secondary bacterial infections. An estimated one in seven COVID-19 patients will develop a secondary infection while hospitalized.
Further, SAB reports that a separate study found that only about 50 percent of patient deaths were due to the original viral infection, while the other 50 percent were caused by subsequent secondary infections.
Even when hospitals observe strict infection-control practices, it’s easy for viral and bacterial co-infections to make their way around, infecting multiple patients living in close quarters and attended to by the same staff.
What’s more, the most severely ill coronavirus patients end up requiring mechanical ventilation, which, although a lifesaving procedure, will exacerbate the risk of bacterial infection when used over long periods.
10 Daily reported on the 12th April 2020 in an article entitled “Doctors Warn Treating Covid-19 Patients With Ventilators Is Doing More Harm Than Good” that as health officials around the world push to get more ventilators to treat coronavirus patients, some doctors are moving away from using the breathing machines when they can.
This is because some hospitals have reported unusually high death rates for coronavirus patients on ventilators, and some medical experts are concerned the machines could be harming certain patients.
Furthermore 10 Daily reports that experts said 40 to 50 percent of patients (in general) with severe respiratory distress die while on ventilators. But 80 percent or more of coronavirus patients placed on the machines in New York City have died, according to state and city officials.
Higher-than-normal death rates also have been reported elsewhere in the US, said Dr Albert Rizzo, the American Lung Association’s chief medical officer. Similar reports have emerged from China and the United Kingdom. In Britain, for instance, that figure is believed to be 66 percent.
Meanwhile, a very small study in Wuhan, the Chinese city where the disease first emerged, said 86 percent died. Apparently the reason is not clear.
Dr Eddy Fan, an expert on respiratory treatment at Toronto General Hospital, said. “We know mechanical ventilation is not benign,” “One of the most important findings in the last few decades is medical ventilation can worsen lung injury — so we have to be careful how we use it.”
“The dangers can be eased by limiting the amount of pressure and the size of breaths delivered by the machine”
It is reported that some doctors say they’re trying to keep patients off ventilators as long as possible, and turning to other techniques instead and increasingly, physicians are trying other measures first including placing patients in a prone position, giving patients more oxygen through nose tubes or other devices and some are experimenting with adding nitric oxide to the mix, to help improve blood flow and oxygen to the least damaged parts of the lungs.
Dr Joseph Habboushe, an emergency medicine doctor who works in Manhattan hospitals said that “If we’re able to make them better without intubating them, they are more likely to have a better outcome, we think,”
The 10 Daily report goes onto report that according to Dr William Schaffner, an infectious diseases expert at Vanderbilt University, there are widespread reports coronavirus patients tend to be on ventilators much longer than other kinds of patients.
For instance, experts believe patients with bacterial pneumonia, may be on a ventilator for no more than a day or two. Whereas according to New York Governor Andrew Cuomo it’s been common for coronavirus patients to have been on a ventilator “seven days, 10 days, 15 days, and they’re passing away,”
Other effects of mechanical ventilation
N. Soni et al British Journal of Anaesthesia 2008 reported that positive pressure ventilation is a radical departure from the physiology of breathing spontaneously.
The immediate physiological consequences of positive pressure ventilation such as haemodynamic changes are recognized, studied, and understood. There are other significant physiological interactions which are less obvious, more insidious, and may only produce complications if ventilation is prolonged. The interaction of positive pressure with airway resistance and alveolar compliance affects distribution of gas flow within the lung.
The result is
• a wide range of ventilation efficacy throughout different areas of the lung, but the pressure differentials between alveolus and interstitium also influence capillary perfusion.
• The hydrostatic forces across the capillaries associated with the effects of raised venous pressures compound these changes resulting in interstitial fluid sequestration.
• This is increased by impaired lymphatic drainage which is secondary to raised intrathoracic pressure but also influenced by raised central venous pressure.
• Ventilation and PEEP promulgate further physiological derangement.
• In theory, avoiding these physiological disturbances in a rested lung may be better for the lung and other organs.
• An alternative to positive pressure ventilation might be to investigate oxygen supplementation of a physiologically neutral and rested lung. Abandoning heroic ventilation would be a massive departure from current practice but might be a more rationale approach to future practice.
Dr Angelo Morella PhD, MRACI CChem, is a Drug Delivery and Pharmaceutical Consultant with over 30 years’ experience in the pharmaceutical industry.














Jeff Curtis
April 25, 2020 at 7:44 pm
I cannot understand why Induced Nitric Oxide – iNOS, in not given more consideration as a form of treatment against COVID-19.
Studies have shown that iNOS can inhibit the Coronavirus by up to 82% [1] , other Studies have shown that iNOS can inhibit the influenza virus and virus infections in general [2,3] and there are studies that have demonstrated that iNOS inhibits Porcine Coronavirus [4]
There seems to be much research done on this in the in the past. Although there seems to be focus at present on trying inhaled nitric oxide as a treatment, Inhaled form of Nitric Oxide may NOT be the way to go, given a study showing it to be ineffective against the influenza virus [5].
Perhaps we should be looking at induced NOS through L-Arginine supplementation or via an intravenous feed? The coronavirus has shown to cause more fatalities in older people 65+.
Older people have low levels of Nitric Oxide in their system [6], and especially if they have other underlying illnesses, at the very least, acute supplementation of nitrates or nitric oxide should be considered.
When you think about it, how effective is inhaled nitric oxide going to be with someone who has an impaired lung function, and that is probably going to be case with most patients by the time this type of therapy is considered, by then it’s just too late.
I would have thought the best approach would be to try and increase the bodies NO levels at the very first sign COVID-19 symptoms become apparent, or even flu symptom for that matter.
I believe we really need to rethink our approach with this, and the above mentioned should be given careful and urgent consideration.
1. https://jvi.asm.org/content/79/3/1966
2. https://jvi.asm.org/content/73/10/8880
3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2327086/
4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2902704/
5. https://www.medsci.org/v09p0157.htm
6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3390088/